- Microorganisms constitute 70 percent of the biomass on Planet Earth.
- Comparatively few species are adapted to colonize human surfaces and form a complex Meta-Organism with manyfold mutual benefits.
- Occasionally, microorganisms may overcome the barriers of the skin and mucosal surfaces and may multiply locally or in multiple sites inside the body. This process is called infection.
- Infections can be caused by bacteria, viruses, parasites, helminths, and fungi.
- Immediately after infection, numerous defense mechanisms of the immune system are activated to combat replication of the microbes.
- There is a balance between microorganism and human defense mechanisms, which may lead to either asymptomatic infection or result in a wide spectrum of symptoms from mild to severe disease and even death.
- The most important factors in the diagnosis of infectious diseases are a careful history, physical examination and the appropriate collection of body fluids and tissues.
- Laboratory diagnosis requires between 2 and 72 hours.
- Wherever possible, antibiotics should only be used when sufficient evidence of efficacy is available. Then, however, they should be used as early as possible and in high doses.
- In addition to everyday hygiene measures, vaccination is the most effective measure to prevent infectious diseases.
- Humans have defense mechanisms against micro-organisms exemplified by the immune system that consists of an unspecific (“innate immunity”) and specific (“adaptive immunity”) arm, leading to an effective response via humoral and cellular mechanisms.
- Innate immunity is activable at any time (skin, tears, ciliae, …). It includes recognition of various chemical patterns on microorganisms. Such chemical structures are detected by macrophages or dendritic cells, which travel to the draining lymph nodes and are presented to cells of the adaptive immune system.
- The adaptive immune system is highly specific against individual microorganisms and directed against non-self-structures. It needs days to weeks to be effective and it induces immune memory, allowing for an immediate defense response upon re-infection.
- As a result of presentation of non-self-structures to the adaptive immune system, highly specific antibodies and cells are generated which may kill/neutralize microbial invaders.
- Currently, antibody responses are the cornerstone to vaccine licensure. Functional antibody tests detecting killing/neutralizing ability are the cornerstone of vaccine-induced immunity. Tests for cell-mediated immunity are also considered.
- Antibody responses to vaccines can be evaluated as
- Geometric Mean Titer (GMT) or Geometric Mean Concentration (GMC)
- Fold-rise pre/post vaccination
- Percentage of study subjects achieving a clinically relevant amount of antibody (“sero-responders”)
- Reverse Cumulative Distributions (RCDs), ideally showing data pre- and post-vaccination.
- Epidemiology contributes to vaccine development and delivery by estimating disease burdens, identifying target populations for immunization, designing clinical trials to show vaccine-induced benefits and risks, and for formulating immunization policy.
- To estimate disease burden, a case definition is needed first. This may have several sets of criteria, depending on how definite the diagnosis is to be.
- Epidemiological studies to determine time, place, and person are referred to as descriptive epidemiology. Epidemiological studies to determine causes and effects are referred to as analytical epidemiology.
- Epidemiological studies may potentially be biased (systemic errors). Bias must be distinguished from confounding (interfering factors that are linked with both, exposure and outcome).
- Vaccine efficacy studies assess causality between vaccination and disease reduction in a prospective cohort design. Participants are assigned to receive vaccine or placebo usually in a double-blind, randomized fashion and efficacy is calculated from incidence reduction during the study period.
- Impact studies are observational studies and encompass e.g., describing disease reduction in a population over time after introduction of a vaccine, as well as cohort studies where vaccine effectiveness is calculated from cohorts in which vaccine administration is only observed.
- Observational studies are timesaving and less costly compared with prospective cohort studies. However, they are prone to various types of bias, e.g. recall bias if exposure status and outcome status are based on the participant's memory.

- Infectious Diseases result from exposure and contact between a host (human being) and an (uninvited) guest (micro-organism).
- Given the fact that billions of micro-organisms are in and around us at any time, overall, infectious diseases are comparatively rare; of the millions of different microbial species, only about 300 are known to cause human diseases.
- Besides exposure and contact, factors on the side of the host (genetic background, environment, underlying diseases and their therapy) and on the side of the micro-organisms (pathogenicity / virulence factors) are necessary to result in an infectious disease.
- “Colonization” means that a micro-organism can attach on skin or mucous membrane for some time or even indefinitely but does not invade host tissue and does not cause any symptoms. Colonizers may even induce an immune response.
- “Infection” is defined as a micro-organism invading through skin or mucous membranes the tissue of a host, leading to no disease (“asymptomatic infection”); or symptomatic disease. It is followed by health, disability, or death. Following the infection, microorganisms may persist in the body for a long time or even for life without causing any symptoms, which is called “latent infection”.
- Infectious diseases may not only be due to pathogenicity factors of a micro-organism, but may also result from (i.) direct destruction of host tissues (e.g., from viral replication); (ii.) the acute host (immune-) response; and from late immune responses resulting in immune-mediated “post-infectious diseases”. Some infections may cause an immune response that is directed against host-tissue, resulting in an “autoimmune-disease”.
- Given the increasing number of microbes, the increasing number of exposures, and the increasing number and fraction of susceptible/predisposed humans, it is obvious that infectious diseases will increase in the future. Vaccines and vaccination may help solve this problem.
- Innate and adaptive immunity generate pathogen-specific antibodies and cells as basis for the efficacy and effectiveness of vaccines: immunity results in protection.
- For almost all currently licensed vaccines, functional antibodies are the most relevant mechanism of action; they work by binding of an antigen, agglutination, neutralization, complement activation and opsonization directed against specific pathogens or toxins.
- Immune memory generated by either infection or vaccine priming allows rapid production of antibodies and immune cells (3-7 days) upon later re-infection or (booster-) vaccination.
- Vaccine-induced immunity may result in protection even in the absence of any measurable specific antibodies at the time of infection – due to memory cells, and due to the effects of T-cells.
- CD4+ T-cells (“T-helper cells”) induce protection largely by cytokine production, CD8+ T-cells can directly or indirectly kill infected or cancerous cells and they can help clear infections.
- While antibodies against vaccine antigens can easily be measured by a variety of methods, testing for specific T-cell immunity is less well standardized and more difficult to perform.
- The term “seroprotection” indicates a serological value (e.g. a titre), associated with protection used for the purpose of vaccine licensure. Measurements of seroprotection can be the percentage of seroresponders, GMTs, fold rise of antibodies or RCD curves.
- In real life, many factors may contribute to individual protection in both, a positive and a negative direction, including factors inherent with the infecting pathogen, epidemiological factors, host factors, and characteristics of the vaccine and vaccination.
- Unlike general public belief, the “failure to vaccinate” is more relevant than “vaccine failures” in a population.
- Vaccines are biological preparations, often made from attenuated or killed forms of microorganisms or fractions thereof.
- They work by stimulating the immune system to produce antibodies and cells directed against a particular organism, mimicking "natural infection".
- Based on their biological and chemical characteristics, vaccines can be categorized into two basic types, "Live-attenuated" (bacterial or viral) vaccines and "inactivated" or "non-live" vaccines.
- Examples of live-attenuated vaccines include: measles-, mumps-, and rubella-, varicella-, yellow fever-, oral polio- (OPV), rotavirus-, ("nasal-spray") live-attenuated influenza- (LAIV), and BCG-vaccine.
- Attenuation results in micro-organisms that may still infect and multiply in humans, but they do not cause disease. Some of these vaccines are associated with life-long immunity.
- Inactivated or non-live vaccines include those against hepatitis A, influenza, pertussis, rabies or the polysaccharide vaccines directed against encapsulated bacteria (Haemophilus influenzae type b, Streptococcus pneumoniae, Neisseria meningitidis).
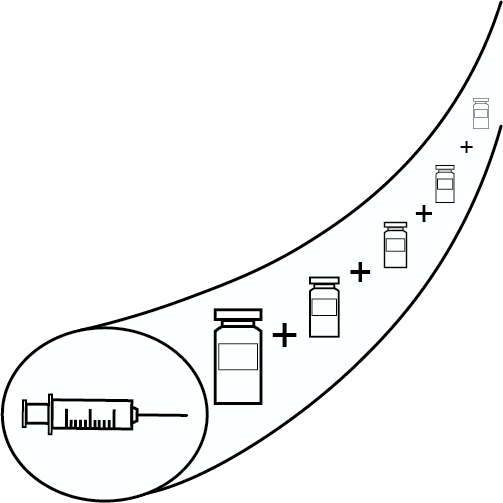
- Most non-live vaccines generally require additional doses ("boosters") to maintain long-term protective immunity.
- There are many other subcategories of these basic groups, like subunit vaccines, whole cell vaccines, toxoid vaccines, polysaccharide vaccines, recombinant protein vaccines, mucosal vaccines, or DNA-, mRNA- and vector-vaccines.
- The concept of developing mRNA as vaccine platform evolved over the last decades. mRNA uses host cells for antigen production, can induce B and T cell responses and does not rely on unwanted antigens that may interfere with booster doses like vector vaccines.
- Unmodified mRNA (uRNA) may be highly reactogenic; modification results not only in improved tolerability but also increases purity and potency. While self-amplifying mRNA (saRNA) leads to higher antigen expression, such constructs are much larger, and this may reduce stability.
- mRNA vaccines need to be formulated in a way that allows cell entry, e.g., by using carefully designed lipid nanoparticles (LNP).
- As response to the COVID-19 pandemic, mRNA vaccines were developed in less than one year from receiving the genetic code to licensure. The 2 marketed and modRNA products widely used today (162b2, Pfizer/Biontech; mRNA-1273, Moderna) differ in vitro in their ability to induce a CD8 T cell response. The development of a third vaccine, based in uRNA, was recently stopped.
- Both licensed modRNA vaccines have an acceptable reactogenicity and safety profile, a protection rate of ≥94% in large double-blind-randomized studies in adults and children ≥12-years of age with a vaccine efficacy against symptomatic disease of >90% in the 6-month follow-up period.
- Viral vector vaccines use harmless, non-replicating or replicating viruses to deliver genetic material for production of vaccine antigens into host cell cytoplasm.
- While viral vector vaccines may theoretically induce life-long immunity with low antigen concentrations, their attenuation, safety and spread to the community are of concern.
- Vaccines based on recombinant viral vectors can induce both humoral and cellular immune responses.
- Adenovirus vectors are versatile gene transfer vectors that can be easily manufactured, and which may allow simultaneous expression of multiple antigens by a single vector construct.
- Adenovirus vector vaccines based on the adenovirus Ad26 vector have been widely used as vaccines against Ebola and COVID19 (see Chapters 44 and 56).
- A common concern of using viral vector vaccines is pre-existing immunity or induction of immunity against the vector itself, but in some circumstances it has no meaningful impact and it can be resolved in several ways.
- Several harmless viruses are already used as vectors for innovative vaccines and many more are in research.
- DNA vaccines were first discovered more than 30 years ago.
- Because DNA vaccines result in antigen production in situ (i.e., mimic a virus infection), they elicit broad-based immune responses, including antibodies and T cells.
- Induction of protective immunity has been established in scores of animal models of infectious and non-infectious diseases.
- Hundreds of human clinical trials have been conducted demonstrating safety and, in many cases, antigen-specific immune responses.
- Several animal health vaccines based on DNA have been approved and are in use.
- Many DNA vaccines are in various stages of human clinical testing, including a few in phase 3 efficacy trials and the recent Emergency Use Authorization of a COVID-19 vaccine, but to date no DNA vaccines have been fully licensed for human use.
- DNA vaccines are thermostable and amenable to large-scale manufacturing at relatively low cost, hence well-suited for global use, particularly in the developing world.
- If potency in humans could be achieved, DNA vaccines would have the potential to be a radical innovation that could disrupt the vaccine industry.
- Adjuvants are present in all vaccines, either as part of the killed or live attenuated pathogens, or added to the vaccine.
- An efficient immune response cannot exist without the antigen and the adjuvant activating together the antigen presenting cells.
- There are more than 10 adjuvants that are part of licensed vaccines.
- They can be tailored to the pathogen, type of immune response expected and targeted population.
- They will continue to be part of vaccines, even for mRNA vaccines as they are already present as part of the mRNA sequence.
- Vaccines contain active ingredients (antigens; mRNA) and inactive ingredients (stabilizers, antimicrobials, inactivating agents, antibiotics, residues of production).
- Formaldehyde is a “natural substance” in human metabolism. With this “natural presence” in mind, the amount of formaldehyde contained in vaccines is not relevant. However, high formaldehyde concentrations in gaseous form may act as a carcinogen.
- Thiomersal was withdrawn from inactivated pediatric vaccines from the year 2000. Available evidence today indicates that it does not cause autism. It has never been an ingredient in live vaccines.
- Penicillin and streptomycin are not used or added during vaccine production, allergies to neomycin are extremely rare.
- Patients with severe hen egg protein allergy (1) can safely be vaccinated with MMR- or TBE-vaccines; (2) should receive egg-protein-free influenza vaccine based on cell culture technology; (3) Yellow fever vaccine is contraindicated, but if necessary, it can be given in graded doses by an allergist.
- Introduction
- Vaccines are biological products that elicit a protective immune response. The details of the manufacturing processes are varied depending on the particular characteristics of the vaccine.
- There are classically, three basic types of vaccines against viral and bacterial pathogens (For mRNA-, DNA- and vector-vaccines see Chapters 7, 8, 9):
- Live-attenuated.
- Killed (non-live).
- Subunit.
- “Classical” Vaccine Production
- The basic classical process includes 5 phases: expression, harvest, inactivation, purification, formulation.
- The expression systems for viral and bacterial vaccines are distinct. Bacterial expression is performed in fermenters. Viral vaccines are produced in animal cell culture or embryonated chicken eggs.
- Processes for whole viral or bacterial vaccines often involve only limited processing after expression.
- Subunit vaccines routinely require the most purification to separate the product from other contaminants.
- Challenges
- Challenges for bacterial vaccines include testing to ensure the safety and efficacy of the product.
- Inactivation procedures need to be carefully controlled.
- Live attenuated vaccines need to be tested to ensure the vaccine strains are still safe and effective.
- Viral vaccines require testing to ensure foreign infectious agents are not introduced during processing.
- Both cultured cells and egg present risks for infection.
- Live viral vaccines and gene vectors need to be carefully engineered and tested to minimize safety concerns.
- Highly variable vaccine targets such as influenza need to be re-adapted to current circulating strains.
- Challenges for bacterial vaccines include testing to ensure the safety and efficacy of the product.

- Vaccine Clinical Development is an integrated part of the overall process of vaccine development, which involves clinical trials in which study participants are usually prospectively and randomly allocated to receive the vaccine candidate or a control vaccine.
- Participants are then actively monitored to generate information on safety, and often immune responses and/or cases of the target disease.
- Clinical development starts with small phase 1 studies in tens or hundreds of volunteers.
- In phase 2, volunteers in the target population are studied for safety and evidence of a desired effect, often an immune response.
- In phase 3, pivotal studies will generally examine prevention of the target disease with at least 3000 participants receiving the vaccine candidate.
- The key outputs are reports for regulatory agencies, policy makers and health care workers to support marketing approval and appropriate ways to use the vaccine.
- Clinical trial designs and results are made public through registries and peer-reviewed publications.
- Clinical trials (a.k.a. clinical studies) in vaccinology are investigations with humans to assess the immunogenicity, reactogenicity i.e., the expected local or systemic symptoms of the desired immune response, safety and/or efficacy or effectiveness of vaccines.
- Such investigations must be designed, conducted, and analysed based on scientific principles to get sound answers to specific questions stated in the trial plan.
- Since Clinical Trials involve human subjects, highest ethical standards need to be applied.
- In addition, national laws, licensing regulations and international standards, for example Declaration of Helsinki, regulate the procedures and conduct of clinical trials.
- Vaccine trials can be classified by development phase (phase I-III before licensure; phase IV post-licensure); by purpose; or role of the investigator.
- The study protocol covers design, selection of study subjects, selection of endpoints, methods to minimize bias, conduct of the study and analysis plan, all aimed at answering the study question with best possible internal scientific validity.

- Vaccines must meet the highest standards for safety and efficacy, as they are used for prevention of diseases in healthy subjects, not as treatment for disease.
- Vaccines are biological products (live or inactivated whole microorganisms or extracts thereof, sometimes heterogenous composition, sensitive to manufacturing conditions, etc.), and thus by their nature they are different from other medicines.
- The licensing process itself – from development and manufacturing to evaluation of safety and effectiveness post licensure – are the product: “Development and production processes are the licensed product.”
- In the USA, licensing granted by the FDA encompasses two phases: an “Investigational New Drug” (IND-) phase” and a “Biologics License Application (BLA-) phase” with defined timelines and procedures.
- There are several ways to accelerate vaccine development and licensing if it is of high public health interest.
- To support licensure, efficacy must usually be shown by disease reduction in high-quality randomized controlled clinical trials (RCTs). Alternatively, licensure can be obtained based on RCTs using a validated “correlate of protection”, or animal studies if human clinical studies are not feasible. A “surrogate of protection” that is reasonably likely to predict clinical benefit may be used to support conditional licensure under the Accelerated Approval pathway with a commitment to conduct a clinical endpoint efficacy study as a post-approval commitment.
- For the European Union (EU) and the three European Economic Area (EEA) states, the European Medicines Agency (EMA) is responsible for vaccine licensure. Here vaccines can be licensed by a (1) Centralized Procedure, (2) Mutual Recognition, (3) Decentralized Procedure, or (4) National Procedure.
- In addition, for licensed vaccines, “WHO prequalification” offers a way to provide existing affordable, safe, and effective vaccines to resource-poor countries.
- Unlike all other medical interventions, vaccine use largely depends on recommendations given by National Immunization Technical Advisory Groups (NITAGs).
- Unlike recommendations of other bodies, NITAGs have overarching public health aspects in mind and usually look at the framework of vaccine use in their respective country, including local epidemiology, vaccination schedules, and finances.
- To be publicly well accepted and trusted, transparency, independence and highest scientific standards are key.
- Quality criteria for NITAGs as set forward by a WHO group are written terms of reference, administrative basis, members hold different areas of expertise, meet ≥1 times per year with agenda and background data distributed in advance, and disclosure of potential conflicts of interest.
- Before NITAG recommendations become effective, various additional and often complicated other local procedures are needed.
- Among the most challenging hurdles NITAGs face are the lack of epidemiology data in many countries, the lack of politically supported vaccines and vaccination goals in short- and in long-term, as well as the lack of local on-time data on vaccine uptake and effectiveness.
- Most countries globally only have NITAG-recommended vaccination plans but no vaccination program including specific goals, responsibility for implementation, and proper science-based current evaluation.
- First vaccines and vaccination schedules were based on “trial and error” and on immunogenicity data (serology).
- Since the 1990s at the latest, vaccination schedules have been based on well-defined phase 1–3 development programs as basis for licensure of any new product.
- Vaccination schedules must bear in mind the epidemiology of the targeted disease; the biology of available vaccine product(s); local opportunities to vaccinate; monitoring for the desired outcome.
- There are 4 basic primary vaccination schedules for children, based on historical development and local needs. Birth doses are recommended with BCG and hepatitis B vaccine.
- Dosing in the 2nd year of life is usually needed for long-term protection induced by polysaccharide-conjugate vaccines.
- Live vaccines (MMR, VZV) are usually given as of 9 months of age – later dosing may induce improved immune responses; a second dose is needed before school entry for optimal protection.
- In addition to “general regular schedules” vaccines and schedules emerge for pregnant women, international travelers, persons above 60 or 65 years, immunocompromised hosts.
- Immunization is a key public health intervention that can help nations attain Goal #3 of the UN Sustainable Development Goals as vaccines already prevent about 2–3 million deaths each year.
- To be effective, immunization services must be designed and delivered in a way to reach populations who need them, irrespective of who they are and where they live.
- Effective national immunization systems must have clear plans based on a vision of the future and a step-by-step process on how the vision will be translated into reality. Such plans are structured around eight topics that go beyond vaccine licensure and recommendations, including management, financing, logistics, human resources, service delivery, vaccine supply and quality, disease surveillance, advocacy and communication.
- The cold chain system is the backbone of any immunization program and consists of a network of equipment, material, people, processes, and financial resources that enable safe transportation of vaccines from the factory to the point of administration to the patient.
- Immunization service delivery includes any strategies and activities for delivering immunization service to a target population.
- Introduction of a new vaccine in a country program requires coordinated decision-making, considering the burden of disease, the characteristics of the respective vaccine and the capacity of the immunization system to deliver it.
- Adverse Events Following Immunization is another key component as documentation of vaccine safety is crucial for trust in a vaccination program.
- Scientifically valid and timely burden-of-disease surveillance as well as vaccine uptake data are core functions of any vaccination program and needed for information of the public and for timely actions.

- Vaccines are extremely effective public health tools which can dramatically improve the health of populations and individuals.
- Physicians who administer vaccines should familiarize themselves with the indications and contraindications of the specific product they use as well as its licensed and recommended dosing and schedules.
- Informed consent must be obtained according to local rules and regulations.
- Manufacturer requirements for shipping, handling, and storage should be followed to assure that the vaccine remains effective and safe for use.
- Different vaccines are administered by different routes – whether ID, SC, IM, or orally. The appropriate route should always be used as per the package insert.
- Vaccines do have side effects; most common are fever and reactions (pain, swelling, tenderness) at the injection site. These are usually mild, transient, and easily treated symptomatically. Providers should counsel vaccine recipients to anticipate such events.
- Care should be taken not to inappropriately attribute adverse events following immunization (AEFIs) to the respective vaccine as AEFIs can occur by chance (without immunization) as well.
- Anaphylaxis can be caused by all vaccines, but it is very rare. However, since it can be rapidly life-threatening, vaccinators must be prepared to treat this emergency.
- Adverse effects may be related, unrelated, or unknown in relation to a vaccine and may range from self-limited mild reactions to permanent sequelae.
- The causal inference of any adverse effect to a vaccine is based on assessing the strength of association, temporal response, consistency and specificity of the association, and biological plausibility.
- Safety evaluation depends on accurate reporting of adverse events during pre-licensure studies and post-licensure surveillance.

- The economic importance of vaccines lies partly in the burden of disease that can be avoided and partly in the competition for resources between vaccines and other interventions. Decision-makers are increasingly demanding hard economic data as a basis for the allocation of limited healthcare resources.
- The main types of evaluation available are cost-benefit analysis (best use of allocated resources), cost-effectiveness analysis (a tool that helps policy-makers decide on the overall allocation of resources), and cost-utility analysis (quality-adjusted life year [QALY] which allows for a direct comparison of a wide range of medical interventions).
- The cost per QALY for a range of vaccinations can be compared in order to plan a vaccination program.
- Public health vaccines warrant a cost-benefit approach, in order to determine if they are worthwhile, whereas recommended vaccines might be more usefully assessed by cost-effectiveness analysis.
- Although cost-savings do not necessarily equate with cost-effectiveness, cost-savings are achieved in many vaccination programs.
- Infectious disease (ID) are a major cause of morbidity and fatality in the ICH and moreover IDs may trigger underlying diseases or graft versus host disease (GVHD) and organ rejection.
- To reduce risk, management of ID in ICH requires a comprehensive management from day 1, with (1) reduction of exposures: fewer social contacts; cocooning (vaccination of any close contacts); appropriate “low pathogen-diet”; avoiding environmental exposures (dust); (2) Detection of pre-existing risks (latent infections, vaccination history); (3) bearing in mind “expected IDs” by type and severity of immunosuppression.
- Inactivated vaccines have similar reactogenicity and safety profiles in the ICH and health subjects; however due to reduced immunogenicity, efficacy may be reduced.
- Live vaccines are usually contraindicated as they may cause harm in severely immunocompromised patients; however, they can be considered based on an individual risk-benefit assessment with remaining immune functions in mind.
- In some instances, post-exposure prophylaxis with immunoglobulins is effective, (“passive immunization”) specifically against measles and the varicella-zoster-virus. For the latter, antivirals can be used as an alternative.

- Due to immunological peculiarities in pregnancy, pregnant women are particularly vulnerable to a number of infectious diseases.
- Vaccinations before conception or during pregnancy can protect pregnant women from infection or severe courses of several vaccine-preventable diseases.
- Transplacental transfer of maternal IgG antibodies (induced by vaccination of the women before or during pregnancy or natural infection) protects the newborn from a variety of diseases in the first months of life.
- Maternal antibodies (mainly IgA) can also be secreted into the breast milk and provide additional protection for breastfed newborns and young infants.
- Inactivated vaccines are generally safe and effective in pregnancy.
- Live-attenuated vaccines are generally contraindicated in pregnancy.
- Routine vaccinations in pregnancy include vaccinations against influenza, tetanus, diphtheria, and pertussis and are recommended in many countries worldwide. In the current pandemic situation, routine vaccination against COVID-19 is recommended for pregnant women as well.
- Pandemics will continue to threaten public health and even mankind; what we have learned from past events has been published manyfold, e.g., by WHO.
- Pathogens with pandemic potential have been identified and, as the “post-pandemic period is the pre-pandemic period”, organizations and structures with the appropriate financial and human resources to prepare for pandemics are needed within a framework of global collaboration.
- Past successes in pandemic preparedness came from decades of multidisciplinary research collaboration and support for basic sciences; thus, to translate innovation into usable products, long-term investments in basic research are essential.
- The “One Health Approach” acknowledges that humans, animals and the environment form an interconnected framework for emerging “new” pathogens that may in the future cross the species barrier. The 2010 Nagoya protocol (UNTC) should be fully implemented.
- Once all of the above points have been considered and implemented, “ad hoc” vaccine production capacities and the logistics for distribution and vaccination need to be readily available.
- Sufficient funding is crucial not only before, but also early on during a pandemic to guarantee that sufficient amounts of life-saving products are available for all populations.
- Regulatory responses allowing rapid evaluation of new vaccines without compromising product safety form another cornerstone for successfully fighting pandemics.
- Pre-pandemic preparedness efforts must be sustained, even if other urgent public health matters need to be addressed today.
- Vaccines in routine use around the world have been shown to be clinically well-tolerated and in double-blind randomized prospective controlled field trials – to be efficacious. Furthermore, they have been proven to be effective in routine vaccination programmes worldwide. They have had an excellent safety profile.
- Vaccinated individuals will face a greatly reduced danger of contracting the targeted disease with a minimal risk of serious side-effects.
- Should the vaccine fail to give complete protection, the severity of the "breakthrough" disease and its accompanying complications will, in most cases, be less than among the unvaccinated.
- Mortality, if a possible outcome, will also be greatly reduced.
- Mass vaccination of children in developed nations have brought many vaccine-preventable diseases under control or even eliminated them.
- Vaccines have made erstwhile lethal infectious diseases so rare that they have become "victims of their own success" to the point that uninformed people query the necessity of continuing to use them.
- Unless a disease is eradicated on a global scale – as has been achieved for smallpox and will soon be for poliomyelitis – vaccination cannot cease since the pathogen will quickly reappear and spread with dire consequences.
- Elimination of disease has many socio-economic, educational, and geo-political advantages.
- Healthy children grow to become well-educated and productive citizens that live longer. Increased life-expectancy brings prosperity and wealth buys health.
- Reduced infant mortality will put a brake on population growth in less developed countries and ease pressure on land and food – a determinant of belligerence.
- Vaccines are a powerful tool to foster equity and peace in the world.

- Vaccine-hesitant individuals are a heterogeneous group that are indecisive in varying degrees – more of a spectrum – about specific vaccines or vaccination in general.
- Vaccine hesitancy is complex, varying by vaccine, time, context, geographic region, and sub-population.
- There is an “infodemic” that needs to be fought alongside the pandemic as exposure to misinformation is linked to a reduction in an individual’s intentions to vaccinate.
- In addressing vaccine hesitancy, it is key to 1) identify the subpopulations susceptible to vaccine hesitancy, 2) diagnose issues through various research methods – surveys, in-depth interviews, focus groups, or media monitoring – and 3) develop context-tailored, evidence-based interventions to address those reasons.
- Sensitivity to the context and effective communication are key to successful immunization programs, alongside other critical factors (confidence, complacency and convenience – the 3Cs model); engaging stakeholders in dialogue is critical to intervention design and implementation.

- Vaccinations are among the most effective and cost-effective means to reduce the burden of serious infectious diseases.
- As vaccination rates remain too low to realize the full potential to reduce morbidity and mortality, strategies to increase immunization rates are ethically and economically mandated.
- Questions to be addressed in this framework are:
- Which restrictions to individual decisions are ethically acceptable in order to achieve a sufficient protection of the community?
- Does the individual have an ethical obligation to get vaccinated?
- Which requirements do vaccines have to fulfill to be ethically acceptable?
- Five criteria are presented:
- Proven efficacy/effectiveness,
- favorable benefit-risk ratio,
- acceptable benefit-cost ratio,
- minimized restrictions of the individual, and
- fair and transparent decision procedures.
- Depending on how far the five ethical requirements are met, different strengths of recommendations result, from level 1 (do not offer vaccination) to level 5 (vaccination required by law).
- Ethical issues on the vaccination of children arise if the human right of parents to care for their child are in contrast to the human right of children to receive optimal protection from disease.
- Combination vaccines have been around since 1945 (trivalent influenza vaccine) and they combine either different serotypes of one microorganism (e.g., influenza or pneumococcal vaccines) or different microorganisms (e.g., DTP combinations).
- Potential chemical and physical interactions, unpredictable immunological interactions, and in one instance: increased AE, increasing likelihood of production failures, and reduced flexibility of a vaccination program are challenges for developing combination vaccines.
- With an increasing number of new vaccines for protecting the very young, DTaP- and DTwP-based combinations have become the cornerstone of pediatric vaccination programs around the globe since the mid-1990s.
- Live vaccine combinations include MR, MMR, and MMRV combinations as well as (trivalent) OPV.
- Combination vaccines for travelers include HAV-HBV combination and HAV-Ty vaccines.
- Dozens of diverse combination vaccine products are licensed today around the globe, some of them only in single countries to cover specific local needs.
- Combination vaccines have been shown to result in increased acceptance, completion and compliance with vaccination programs; in addition, they offer simplified logistics, reduce administration errors, reduce the number of medical visits and cost for the individual as well as for society, among other benefits.